What Are Testicles For?
The testes produce and store sperm, and are also the body's main source of male hormones, such as testosterone. These hormones control the development of the reproductive organs and other male characteristics, such as body and facial hair, low voice, and wide shoulders.
The testes are located in the scrotum, a sac or pouch that hangs outside the main body. This external location allows the testicles to have a temperature about 4°C cooler than the core body temperature which seems to be optimal for sperm development.
Seminiferous tubules, the coiled, hollow tubes in which sperm are produced nearly fill each of the testes. In spaces in between the tubules are the Sertoli cells, which synthesize testosterone.
Just inside the wall of each seminiferous tubule lie the spermatogonia and Sertoli cells. Both are diploid cells.
When spermatogonia divide they can either undergo mitosis and produce more spermatogonia or they can undergo meiosis and produce spermatocytes which differentiate into sperm cells. Sperm cells, remember, are haploid cells.
Sertoli cells regulate the process of spermatogenesis and nourish the developing sperm cells.
A human sperm cell is unlike any other cell in the body. Most of its cytoplasm is lost. It consists largely of a nucleus, mitochondria and a flagellum. At the tip of the sperm cell is a specialized lysosome called an acrosome. The acrosome contains specialized enzymes necessary for penetration of the egg cell.
Sperm production does not begin until puberty. At that time, the hypothalamus releases a hormone, gonadotropin-releasing hormone, that stimulates the anterior pituitary gland to produce luteinizing hormone and follicle-stimulating hormone.
Spermatogenesis begins as a result of the interplay of luteinizing hormone, follicle-stimulating hormone and testosterone (the latter secreted by the testes).
Luteinizing hormone stimulates the interstitial cells of the testes to produce testosterone. The combination of testosterone and follicle-stimulating hormone stimulates the Sertoli cells and spermatogonia, causing spermatogenesis.
Let me go over this sequence again, this time inserting feedback control notions. Gonadotropin-releasing hormone from the hypothalamus stimulates the anterior pituitary to release luteinizing hormone and follicle-stimulating hormone. Luteinizing hormone stimulates the interstitial cells of the testes to produce testosterone. Follicle-stimulating hormone stimulates the Sertoli cells and the spermatogonia to undergo spermatogenesis. Testosterone and chemicals produced during spermatogenesis inhibit further release of luteinizing hormone and follicle-stimulating hormone, forming a negative feedback loop that keeps the rate of spermatogenesis and the level of testosterone in the blood nearly constant.
Testosterone also stimulates the development of secondary sexual characteristics such as the growth of facial hair in males. It maintains sexual drive and is absolutely required for successful sexual intercourse or copulation by the male.
Interestingly, sperm are not involved in these functions. If one could suppress the production of follicle-stimulating hormone (which would block spermatogenesis) BUT allow the release of luteinizing hormone (which would allow the production of testosterone), a man would be infertile but not impotent. Birth control where the male is the controlled individual would be the result.
Sperm is not semen. The seminiferous tubules merge near the top of the testicle to form a structure called the epididymis. This becomes the vas deferens which leaves the scrotum and enters the abdominal cavity. Most of the hundreds of millions of sperm produced each day are stored in the vas deferens and epididymis.
The vas deferens joins the urethra which moves to the tip of the penis.
The fluid ejaculated from the penis is semen, a mixture of sperm cells, and secretions from the seminal vesicles, the prostate gland and the bulbourethral glands. These secretions activate the sperm into swimming structures and neutralize the acidic fluids of the vagina that normally inhibit bacterial growth.
Common testicular problems
Testicular cysts
* a cyst is a collection of fluid. A cyst around the testis is called a hydrocoele
* usually painless
* may develop as a result of injury or infection of the testis or epididymis
* can be very large
Treatment may involve draining fluid out of the cyst with a needle or, surgical removal with an anaesthetic.
Infection of the testes
* can affect men of any age
* main symptoms will usually be pain or inflammation of the testes,
and fever with infections
Infections may be caused by a sexually transmitted disease, a urinary tract infection or even mumps. There may be a fever, and the testes may become red and sore. Treatment usually involves bed rest, wearing scrotal support and taking painkillers or a long-term course of antibiotics.
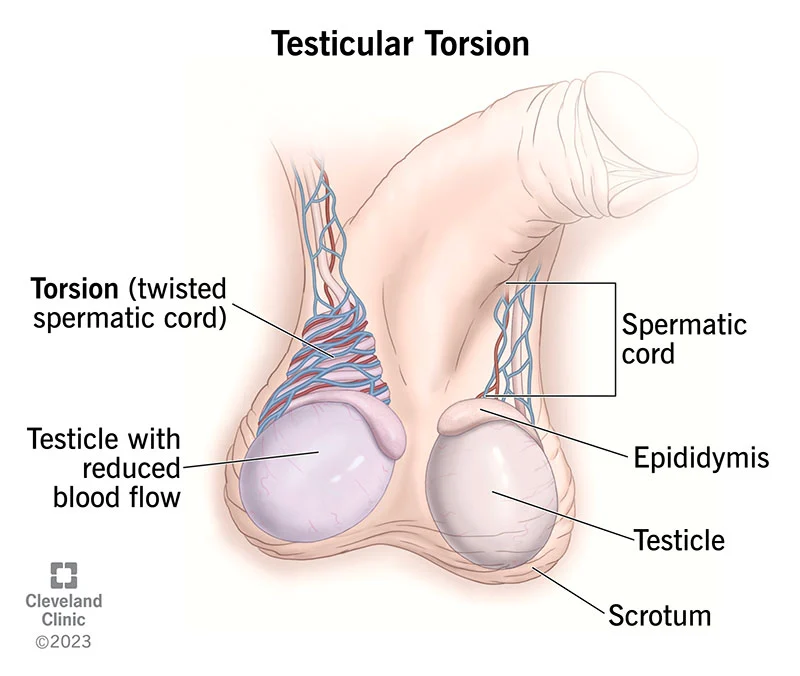
Torsion of the testis
- Can occur at any age, but is most common in babies, and in men between 13 and 16 years
- Often as a result of sporting activity
Torsion of the testis happens when the spermatic cord gets twisted, making it impossible for blood to flow normally to the testis. Severe pain is the main symptom, and the testis may become red and swollen. If you suspect you have a torsion, get medical advice immediately. If left for even a few hours it may result in permanent damage and the testis may have to be removed. Treatment usually involves an emergency operation to untwist the testis, so that the blood supply returns to normal. To prevent the chance of torsion recurring, the surgeon will stitch the testes into place in the scrotum during the operation.
Testicular cancer
* the most common form of cancer in young men
* usually occurs between the ages of 15 and 49
* still quite rare, with just over 1,500 new cases each year
The cause is not known, but about 10 per cent of malignancies appear to be a consequence of the testes not descending properly into the scrotum in childhood. Other research suggests a hereditary factor - especially if your father or a brother has had the condition. Over 90 per cent of patients make a complete recovery, and when caught early enough, the cure rate for this cancer is almost 100 per cent (Source: Imperial Cancer Research Fund).
Treatment normally involves:
* surgical removal of the diseased testis
* radiotherapy (cancer-killing X-rays) or chemotherapy (cancer-killing drugs) may be recommended by the doctor in addition to surgery